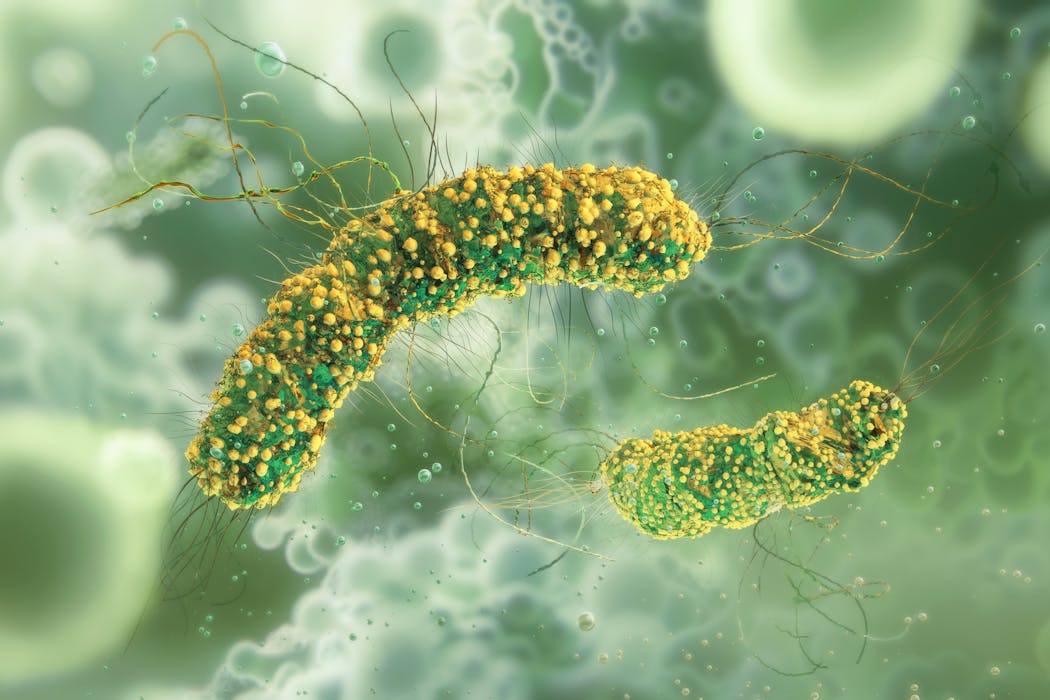
Bacteria are rapidly emerging as a new class of “living medicines” used to kill cancer cells.
We’re still a long way from a “cure” for cancer.
But one day we could have programmable, self-navigating bacteria that find tumours, release treatment only where needed, then vanish without a trace.
Here’s where the science is up to.
Current treatments aren’t perfect
Many tumours are hard to treat. Sometimes, treatments cannot penetrate them. Other times, tumours can “fight back” by suppressing certain parts of the immune system, reducing the impact of treatments. Or tumours can develop resistance to treatments.
Using bacteria could overcome these obstacles.
More than a century ago, surgeons noticed some people with cancer who developed bacterial infections unexpectedly went into remission. That is, their cancer signs or symptoms decreased or disappeared.
Now we’re learning what could explain this. Broadly speaking, bacteria can activate the body’s immune system to attack cancer cells.
In fact, this approach is already used in the clinic. Bacteria are now the treatment of choice worldwide for certain cases of bladder cancer. When doctors deliver a weakened version of Mycobacterium bovis directly into the bladder through a catheter, the body’s immune response destroys the cancer.
Why bacteria?
Certain bacteria have an unusual talent. They can naturally find and grow inside solid tumours – ones that grow in organs and tissues – but leave healthy tissue relatively untouched.
Solid tumours are perfect homes for these bacteria as they contain lots of nutrients from dead cells, are low in oxygen (an environment these bacteria prefer), and typically have reduced immune function, so cannot defend themselves against the bacteria.
All this suggests possible careers for these bacteria as delivery couriers to carry targeted, anti-tumour therapies.
Over the past 30 years or so, more than 500 research papers, 70 clinical trials and 24 startup companies have focused on bacterial cancer therapy, with growth accelerating sharply in the past five years.
Most bacterial cancer therapies in clinical trials today target solid tumours, including pancreatic, lung, and head and neck cancers, which are the kinds that often resist conventional treatments.
Bacteria could deliver cancer vaccines
Cancer vaccines work by presenting a cancer’s unique molecular “fingerprints”, known as tumour antigens, to the immune system so it can hunt down and eliminate tumour cells displaying those antigens.
Bacteria can serve as couriers for these anti-cancer vaccines. Using genetic engineering, the genetic instructions (or DNA) in bacteria that might make us unwell can be removed and replaced with DNA for immune-stimulating tumour antigens.
Listeria monocytogenes is the main character in more than 30 cancer vaccine clinical trials. Unfortunately, most of these trials did not show that these treatments work better than current ones.
The challenge is teaching the immune system to recognise cancer’s telltale antigens strongly enough to remember them, without pushing the body into dangerous overdrive.
Bacteria could boost existing cancer therapies
Nearly half of current clinical trials using bacteria in cancer therapies pair bacteria with immunotherapies or chemotherapy as part of personalised treatment plans to enhance the body’s attack on cancer.
Various approaches have finished phase 2 clinical trials. These include using immunotherapy combined with modified Listeria to activate the immune system for recurrent cervical cancer.
Another trial used modified Salmonella in people with advanced pancreatic cancer alongside chemotherapy to increase survival.
Bacteria could be ‘bugs as drugs’
Arming bacteria with a drug means they could destroy the tumour from the inside, creating “bugs as drugs”.
For this, we need precise genetic control over how bacteria behave. Researchers can already reprogram bacteria to sense, compute and respond to molecular signals around the tumour.
Researchers can also engineer bacteria to self-destruct after delivering a drug, secrete immune-boosting molecules, or activate other therapies on command.
Researchers are building “multi-function” strains that combine several treatment strategies at once.
Probiotic species used in humans for many years are also candidates, including Escherichia coli Nissle, Lactobacillus and Bifidobacterium. These can be engineered to produce cancer-killing molecules or alter the environment around the tumour.
How close are we, really?
While early human trials have shown this approach is generally safe, finding the right dose remains a delicate balance.
Bacteria are also living entities that can evolve in unpredictable ways, and their use in humans demands strict safety controls. Even strains modified for safety can cause infection or trigger excessive inflammation.
So scientists are developing “biocontainment” strategies – engineered safeguards that prevent bacterial spread beyond tumours or triggers them to self-destruct after treatment.
If we can overcome these issues, such “living medicines” would still need to successfully complete clinical trials and receive regulatory approval before being commonly used in the clinic.
If so, this could mark a profound shift in how we treat cancer, from static drugs to adaptive biological systems.
This article is republished from The Conversation, a nonprofit, independent news organization bringing you facts and trustworthy analysis to help you make sense of our complex world. It was written by: Josephine Wright, South Australian Health & Medical Research Institute and Susan Woods, South Australian Health & Medical Research Institute
Read more:
- Scientists are uncovering serotonin’s role in cancer – here’s what we know
- Here’s why morning exercise feels so hard
- We studied 217 tropical cyclones globally to see how people died. Our findings might surprise you
Susan Woods receives funding from the National Health and Medical Research Council, Gastroenterological Society of Australia Bushell Research Fellowship, Faculty of Health Science at the University of Adelaide, Tour de Cure, The Hospital Research Foundation. She has equity in GenCirq Inc, a biotechnology company that engineers bacteria to treat cancer. The company was not involved in clinical trials mentioned in this article.
Josephine Wright does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.


 The Conversation
The Conversation
 Local News in New Jersey
Local News in New Jersey NBC News
NBC News Associated Press US News
Associated Press US News Associated Press Top News
Associated Press Top News Raw Story
Raw Story FOX 32 Chicago Sports
FOX 32 Chicago Sports People Top Story
People Top Story The Daily Beast
The Daily Beast The Times of Northwest Indiana Crime
The Times of Northwest Indiana Crime